Landmark COVID-19 vaccine trial in sub-Saharan Africa
10th January 2022


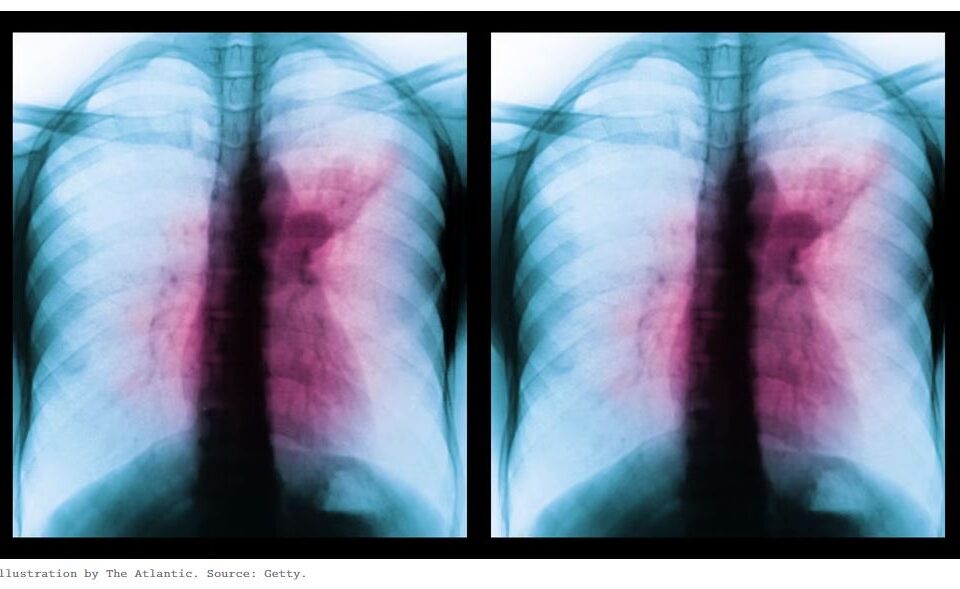
The intersecting pandemics of tuberculosis and COVID-19: population-level and patient level impact, clinical presentation, and corrective interventions
23rd March 2022

Photo Copyright © 2022 Photo taken by staff at the Centre for Lung Infection and Immunity and provided courtesy of Keertan Dheda
Globally, there were about 10 million new cases of active tuberculosis in 2020 and an estimated 1·5 million deaths. In the same year, in many African countries, there were more deaths from tuberculosis than from COVID-19.
Early detection and effective treatment is the key strategy to combat tuberculosis. Unfortunately, even before 2020, about a third of people newly ill with tuberculosis remained undetected—the missing tuberculosis diagnoses.
Detecting these individuals with active tuberculosis is important not only to prevent morbidity and mortality but also to subvert amplification of this airborne epidemic, since almost a third of these people are likely to be highly infectious with smear-positive or cavitory disease.
Indeed, for example, a 2018 South African national door-to-door survey showed that 58% of people with culture-positive tuberculosis did not report any symptoms.
Currently deployed global and national health strategies are not fundamentally configured to detect this missing burden of disease, because they rely on patients self-reporting to clinics or health-care facilities (passive case finding). All these considerations also apply to the multidrug-resistant tuberculosis epidemic response.
COVID-19 was associated with an estimated increase in the number of missing new tuberculosis diagnoses to about 4 million worldwide in 2020. The COVID-19 pandemic has disrupted access to tuberculosis services, resulting in multidimensional effects, including increased tuberculosis morbidity and mortality.However, the scientific and public health response to COVID-19 has also brought many lessons. Within months of the advent of COVID-19, in tandem with massive investments in research and development and ratification of global treaties, new diagnostics, drugs, and vaccines were developed and rolled out on an unprecedented scale.
Why has this response not occurred for tuberculosis? Tuberculosis typically kills over months to years with individuals from marginalised communities dying at home or in outlying hospitals. More than 98% of people who die from tuberculosis live in countries where the majority are people of colour. The disease is also associated with resource limited or historically neglected populations—euphemisms for medical racism—fuelled by structural violence and entrenched systems of socioeconomic exploitation. Investment in the global public sector research and development funding for tuberculosis grew from a pitiful US$389 million in 2010 to a shameful $642 million in 2020. In stark comparison, about $104 billion was spent by governments on research and development in the first 11 months of the COVID-19 pandemic.
Although newer tuberculosis diagnostics, such as GeneXpert Ultra,and newer drugs, such as bedaquiline and pretomanid, have been rolled out slowly, a tuberculosis vaccine with about 50% efficacy has not yet started enrolling patients for phase 3 evaluation 8 years after the phase 2b trial began.This pace, compared with COVID-19 vaccine trials, can only be described as glacial...
Download the PDF