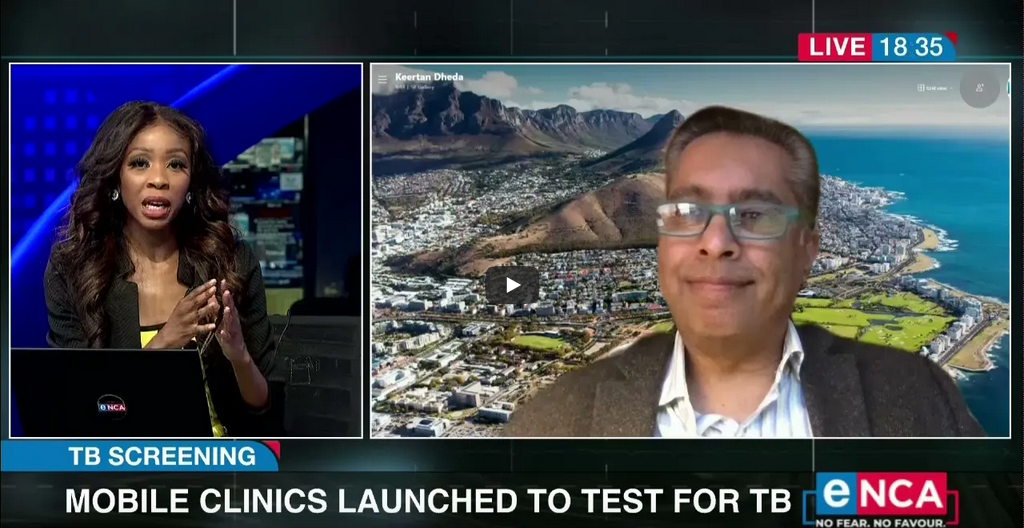
TB Screening | Mobile clinics launched to test for TB
28th March 2021
After setbacks, rollout of new TB prevention pills to start in six districts
14th April 2021Sunday Times DAILY – Tanya Farber – 12 April 2021 – 19:45
Relax when outdoors, say experts, with Irish analysis revealing that only one in 1,000 infections is acquired outside

Image: Supplied
As SA waits for its Covid-19 vaccine rollout to start, new evidence suggests the best weapons in our preventive arsenal are free and plentiful: fresh air and good ventilation.
A study at the US’s University of Central Florida (UCF) says ventilation in classrooms and other indoor settings is even more important than social distancing and an analysis of contact-tracing in Ireland discovered that only one in 1,000 infections is acquired outdoors.
A study in China found poorly ventilated spaces are a top culprit in the rapid spread of the disease. The University of Hong Kong found 10 people from three families got Covid-19 within just a few minutes by sitting at adjacent tables in a poorly ventilated restaurant in Guangzhou.
Pulmonologists at the University of Cape Town (UCT) are also contributing to the body of knowledge of aerosolised transmission, or the spread of the disease by tiny particles that remain suspended in the air after someone exhales.
Prof Keertan Dheda, UCT’s head of pulmonology, told Sunday Times Daily this week: “We have recruited our five first patients. We get them to breathe out into special equipment which allows us to fractionate the particles so we can measure the tiniest of particles, which are less than five to 10 microns in size. We can tell whether they carry the virus and then conclusively prove if it is infectious.”
Aerosols, unlike large respiratory droplets that fall quickly, “remain suspended in the air for minutes to hours, and if you breathe in that aerosol that contains a virus, it is also a mechanism of spread”.
Dheda said ventilation is a fundamental part of preventive protocols. For example, stating that an indoor venue is only allowed 50% occupancy is a weak prevention tool if there is poor ventilation.
“It’s not just as simple as how many people are in the room. If they are all standing in a group and there is poor ventilation and people aren’t wearing masks, it won’t work,” he said, adding that ventilation needs to be emphasised as much as social distancing and masks.
Opening windows and doors is an effective way of providing good ventilation not just for Covid-19 prevention, but tuberculosis too.
Prof Keertan Dheda, UCT’s head of pulmonology
“Opening windows and doors is an effective way of providing good ventilation not just for Covid-19 prevention, but tuberculosis too,” he said, adding that experiments have shown aerosols remain suspended in the air and that there have been cases of people contracting Covid-19 in places such as restaurants and churches despite social distancing.
The study by UCF, published in Physics of Fluids, emphasises the use of masks and good ventilation.
“The research is important as it provides guidance on how we are understanding safety in indoor environments,” said researcher Michael Kinzel.
“The study finds that aerosol transmission routes do not display a need for six-feet social distancing when masks are mandated,” he said. “So these results highlight that with masks, transmission probability does not decrease with increased physical distancing, which emphasises how mask mandates may be key to increasing capacity in schools and other places.”
Masks were shown to be beneficial by preventing direct exposure to aerosols, as masks provide a weak puff of warm air that causes aerosols to move vertically, thus preventing them from reaching adjacent people, Kinzel said.
Additionally, a ventilation system in combination with a good air filter reduced the infection risk by 40 to 50% compared with a classroom with no ventilation.
Prof Simon Clarke, from the University of Reading in the UK, was quoted in The Times there as saying the Irish contact-tracing data “was yet more evidence that people should be relatively relaxed about outdoor activities that have attracted criticism in the past, such as going to the beach”.
But how do you know if ventilation indoors is sufficient to stop the spread?
According to new research at the University of Colorado Boulder in the US, it’s as simple as this: if you track carbon dioxide levels indoors, you can monitor the risk of people getting Covid-19.
“Infectious people exhale airborne viruses at the same time as they exhale carbon dioxide. That means CO2 can serve as a ‘proxy’ for the number of viruses in the air,” said researcher Jose-Luis Jimenez, “In any given indoor environment, when excess CO2 levels double, the risk of transmission also roughly doubles.”



